Abstract
BACKGROUND
Respiratory failure syndromes are common after allogeneic hematopoietic cell transplantation (allo-HCT), and are associated with substantial morbidity and mortality. These syndromes are incompletely understood, and may be associated with histopathologic evidence of acute lung injury (ALI). The role of biopsy in this setting is controversial, with uncertain benefits and considerable procedural risk. We report the clinical, radiologic and histopathologic features of patients with biopsy-proven ALI following allo-HCT in a large multi-site retrospective series.
METHODS
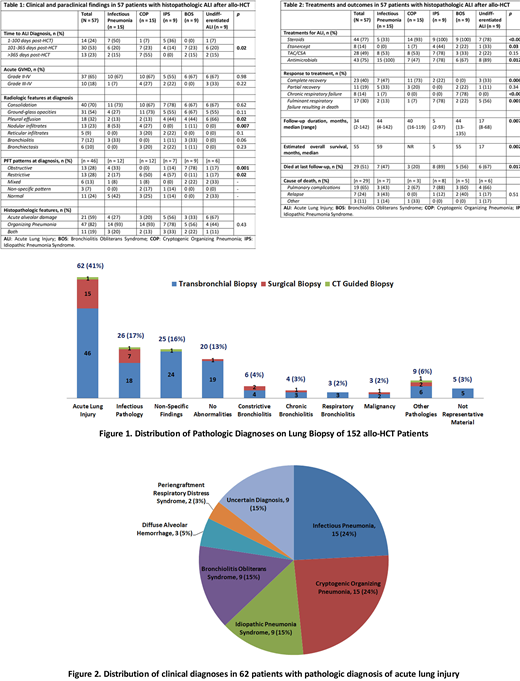
The medical records of 1,864 consecutive adults who underwent allo-HCT at Mayo Clinic, Minnesota (n = 916), Arizona (n = 694), and Florida (n = 254) (Jan 2005-Dec 2017) were reviewed. A total of 152 patients underwent a lung biopsy: 126 bronchoscopic, 22 surgical, and 4 CT-guided biopsies (Figure 1). Patients with a histopathologic diagnosis of ALI were included in the study, and were classified into clinicopathologic subgroups per published American Thoracic Society guidelines (Am J Resp Crit Care Med, 2011). Patients whose diagnosis remained uncertain after a detailed review of the medical records were included in a separate subgroup as undifferentiated ALI. Transplant characteristics, radiologic features, pulmonary function test (PFT) results, treatments, and outcomes were compared between groups.
RESULTS
Clinicopathologic diagnoses in 62 patients with biopsy-proven ALI consisted of an infectious etiology in 15 (24%), cryptogenic organizing pneumonia (COP) in 15 (24%), idiopathic pneumonia syndrome (IPS) in 9 (15%), bronchiolitis obliterans syndrome (BOS) in 9 (15%), diffuse alveolar hemorrhage in 3 (5%), periengraftment respiratory distress syndrome in 2 (3%), and undifferentiated ALI in 9 (15%) patients (Figure 2). Transplant characteristics were comparable between groups. Infectious pneumonia and IPS were the most common diagnoses during the first 100 days post HCT (50% and 36%, respectively). Between 100 and 365 days, a range of diagnoses were seen including infectious pneumonia (20%), COP (23%), IPS (14%), BOS (23%), and undifferentiated ALI (20%) (Table 1). In 14/15 (93%) infectious pneumonia cases, biopsy did not change management and diagnosis was concurrently established by bronchoalveolar lavage (BAL) or non-invasive testing.
Patients with IPS, BOS, and undifferentiated ALI more commonly had a pleural effusion (66%, 44%, and 44%, respectively). Nodular infiltrates were most commonly seen in patients with infectious pneumonia (55%). Other radiographic findings were not clearly discriminative. BOS and infectious pneumonia were more commonly associated with an obstructive PFT (78% and 33%, respectively), whereas restrictive pattern was more frequently seen in COP and IPS (50% and 57%, respectively) (Table 2). Despite a histopathologic diagnosis of ALI, 9 (15%) patients had clear clinical and radiographic evidence of BOS.
Steroids were used commonly in noninfectious syndromes: 93% of patients with COP and in 100% of IPS patients. Of 4 patients with IPS who received Etanercept, 2 (50%) showed complete recovery, whereas the remaining 5 patients who did not receive Etanercept died from fulminant respiratory failure. Most common treatment response was complete recovery in COP (73%), fulminant respiratory failure leading to death in IPS (78%), and chronic respiratory failure in BOS (78%). Estimated OS was shortest in the group with IPS and undifferentiated ALI (median 5 and 17 mons, respectively), whereas patients with COP had the best prognosis (mOS not reached) followed by the infectious pneumonia and the BOS groups (mOS of 59 and 55 mons, respectively). Pulmonary complications were the most common cause of death in patients with non-infectious ALI. Lung biopsy was associated with post-procedural pneumothorax in 17 (27%) patients; 12 of whom required a chest tube.
CONCLUSIONS
In this largest case series to date of histopathologic ALI after allo-HCT, biopsy does not appear to meaningfully change management in the majority of patients, and is associated with substantial procedural risk. Histopathologic findings do not clearly correlate with the clinical and radiographic picture in a sizeable proportion of the patients. PFT results, BAL findings, the timing of the onset of respiratory failure after HCT, and the response to steroids seem to be of greater diagnostic and/or prognostic value.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal